Ventilator is a mechanical breathing aid use to help patients with airway disorders, patients with PaCO2> 50 mmHg and PaO2 <50 mmHg requiring help one of them with ventilator breath.
Things to note on the ventilator:
1. Prisoners airway resistance
2. Komplience lung
3. The desired air volume (flow rate)
4. Humidifier
5. Inspired fractional oxygen consentration (FiO2)
6. Sigh
7. Positive End expiratory Pressure
8. The highest expiratory pressure (pressure Peek Limit)
9. Inspiration and expiratory ratio (I / E ratio)
Steps ventilator settings
1. After intubation followed by mechanical pumps
2. See whether elevated asymmetrical chest wall every time inspiration is given and no air leakage sound
3. Select the mode appropriate ventilator patient's condition
4. At the beginning of the use of ventilators provide FiO2 100%, to maintain SatO2> 92%. FiO2 can be derived after the confirmation of the value of oxygen saturation
5. Given tidal volume 8-10 ml / kg, in patients with acute respiratory failure due to neuromuscular disease often membiutuhkan tidal volume of 10-12 ml / kg
6. Determine the rate of breathing and minute ventilation according to clinical state of patients depending on blood pH
7. Use PEEP in diffuse lung damage, PEEP> 15 cmH2O is rarely necessary.
8. High Pressure inspiration PIP> 60 cmH2O, inspiration plateau pressure> 35 cm H2O must be considered
9. If the ventilator requires a flow rate, use the appropriate flow rate to avoid rapid respiration and autoPEEP
10. If there is difficulty in oxygenation, ventilation or excessive high-pressure inspiration, use appropriate medications or change in position
11. Call critical care consultant.
Selasa, 22 Februari 2011
Health Care Information System
The need for evaluation
Health care organizations-long time uses of computers-are considering many new computer based products in the hope of increasing efficiency, reducing costs, and improving patient care. These products include a growing number of medical computer applications in which health care providers interact directly with the computer. These applications are referred to generally as medical or clinical information systems. Medical information systems involved computer-stored database containing patient information to support medical order entry, result reporting, decision support systems, clinical reminders, and other health care applications. In some health care organizations, a comprehensive systems coordinates patient care activities by linking computer terminals in patient care areas to all departments through a central or integrated information system. Other organizations use smaller separate systems tahat link patient care areas to only one department such as the laboratory, radiology, or the pharmacy. These systems provide communication network between departments as well as storage and retrieval of medical information. Other computerized database or expert systems may serve a single department or group of practitioners.
At the same time, the current emphasis on cost-effectiveness in health care is creating new pressures on organizations to justify expenditures through detailed evaluations of the impacts of new informations systems. Although implementation success depends heavily on the integration of the computer systems into a complex organizational setting, professionals who develop, implement, and evaluate health care computer systems have few guidelines for designing effective evaluation strategies and selecting appropriate methods to examine the outcomes of systems use in health care organizations. To ensure that newly adopted systems accomplish their intended purpose, vendors and purchasers alike need to develop detailed plans prior to system implementation for ongoing implementation and post-instalation evaluation to examine the use and long-term impacts ofthese systems.
Evaluating the impact of computer based medical information systems requires not only an understanding of computer technology but also an understanding of the social and behavioral processes that affect and are affected by the introduction of the technology into the practice setting. As technological developments result in the widespread use of computer in health care, the social and behavioral sciences can provide an important perspective to guide the establishment of research agendas and the conduct of policy-relevant investigations.
Health care organizations-long time uses of computers-are considering many new computer based products in the hope of increasing efficiency, reducing costs, and improving patient care. These products include a growing number of medical computer applications in which health care providers interact directly with the computer. These applications are referred to generally as medical or clinical information systems. Medical information systems involved computer-stored database containing patient information to support medical order entry, result reporting, decision support systems, clinical reminders, and other health care applications. In some health care organizations, a comprehensive systems coordinates patient care activities by linking computer terminals in patient care areas to all departments through a central or integrated information system. Other organizations use smaller separate systems tahat link patient care areas to only one department such as the laboratory, radiology, or the pharmacy. These systems provide communication network between departments as well as storage and retrieval of medical information. Other computerized database or expert systems may serve a single department or group of practitioners.
At the same time, the current emphasis on cost-effectiveness in health care is creating new pressures on organizations to justify expenditures through detailed evaluations of the impacts of new informations systems. Although implementation success depends heavily on the integration of the computer systems into a complex organizational setting, professionals who develop, implement, and evaluate health care computer systems have few guidelines for designing effective evaluation strategies and selecting appropriate methods to examine the outcomes of systems use in health care organizations. To ensure that newly adopted systems accomplish their intended purpose, vendors and purchasers alike need to develop detailed plans prior to system implementation for ongoing implementation and post-instalation evaluation to examine the use and long-term impacts ofthese systems.
Evaluating the impact of computer based medical information systems requires not only an understanding of computer technology but also an understanding of the social and behavioral processes that affect and are affected by the introduction of the technology into the practice setting. As technological developments result in the widespread use of computer in health care, the social and behavioral sciences can provide an important perspective to guide the establishment of research agendas and the conduct of policy-relevant investigations.
Anatomy Retina
The retina is a thin sheet of nerve tissue that semitransparan, and multilapis and line the inside of two thirds of the posterior wall of the eyeball. The retina is often called the retina, is part of the eye contains receptors that receive light stimuli.
Bounded by the choroid and retina pigment epithelial cells of the retina, and consists of layers, ranging from the inside, is as follows:
1. Internal limitans membrane
2. Layer of nerve fibers
3. Layer of ganglion cells
4. Pleksiform layer in
5. In the nuclear layer
6. Pleksiform outer layer
7. Outside the nuclear layer
8. Internal limitans membrane
9. Photoreceptor layer
10. Pigment epithelial layer
In the middle there is the posterior retina macula. In clinical can be defined as an area of yellowish pigmentation caused by luteal pigment (xantofil), and bordered by arcades-temporal retinal vascular arcades. In the middle of the macula, approximately 3.5 mm lateral to the optic disc, fovea that clinically there is clearly a reflection of a basin that provides specially when done oftalmoskop.
Fovea is marked with the depletion layer and the outer core and the absence of the layers of parenchyma because of photoreceptor cell axons run in a centrifugal oblique and shifting layers of the retina that is closer to the surface of the retina. Foveola is the most central part of the fovea, here fotoreseptornya are cone cells and is the thinnest part of the retina.
On funduscopic the macula lutea appear redder than its surroundings and on the central fovea as if no light reflex, called the fovea, which is caused by the curvature at the central fovea. In the nasal part of macula lutea contained Nervi optisi papilla, which is a place where N. II through the sclera. Papil is only composed of nerve fibers, did not contain stem cells or cone at all and called the blind spot.
Indentation in the middle there that looked a little pale, from where this is out of central retinal artery and vein which then ramify into the temporal and the nasal, as well as upwards and downwards. The artery is a terminal artery and no anastomose. But sometimes in to anastomose between a. Siliaris and a. Central retina, called a. Silioretinal located in the macula, so that in case of emboli that enter the central retinal artery of macular function undisturbed.
Suppliers main artery to the orbit and their parts derived from arterial oftalmika, the first major branch of the intracranial internal carotid artery. This branch runs below the optic nerve and optic canal with him through to the orbita. The first intraorbital branch is the central retinal artery, which enter the optic nerve about 8-15 mm behind the eyeball. Retinal blood vessels out in papil N. II, forming a picture of the different branches on each individual.
The retina receives blood from two sources. Usually the inside of the retina is supplied by central and branch a.retina memperdarahi inner two thirds. On the outside is supplied by koriokapiler which is right outside the Bruch membrane, which memperdarahi outer third of the retina. Includes outer layer pleksiformis and outer core layer, photoreceptors, and retinal pigment epithelial layer.
Bounded by the choroid and retina pigment epithelial cells of the retina, and consists of layers, ranging from the inside, is as follows:
1. Internal limitans membrane
2. Layer of nerve fibers
3. Layer of ganglion cells
4. Pleksiform layer in
5. In the nuclear layer
6. Pleksiform outer layer
7. Outside the nuclear layer
8. Internal limitans membrane
9. Photoreceptor layer
10. Pigment epithelial layer
In the middle there is the posterior retina macula. In clinical can be defined as an area of yellowish pigmentation caused by luteal pigment (xantofil), and bordered by arcades-temporal retinal vascular arcades. In the middle of the macula, approximately 3.5 mm lateral to the optic disc, fovea that clinically there is clearly a reflection of a basin that provides specially when done oftalmoskop.
Fovea is marked with the depletion layer and the outer core and the absence of the layers of parenchyma because of photoreceptor cell axons run in a centrifugal oblique and shifting layers of the retina that is closer to the surface of the retina. Foveola is the most central part of the fovea, here fotoreseptornya are cone cells and is the thinnest part of the retina.
On funduscopic the macula lutea appear redder than its surroundings and on the central fovea as if no light reflex, called the fovea, which is caused by the curvature at the central fovea. In the nasal part of macula lutea contained Nervi optisi papilla, which is a place where N. II through the sclera. Papil is only composed of nerve fibers, did not contain stem cells or cone at all and called the blind spot.
Indentation in the middle there that looked a little pale, from where this is out of central retinal artery and vein which then ramify into the temporal and the nasal, as well as upwards and downwards. The artery is a terminal artery and no anastomose. But sometimes in to anastomose between a. Siliaris and a. Central retina, called a. Silioretinal located in the macula, so that in case of emboli that enter the central retinal artery of macular function undisturbed.
Suppliers main artery to the orbit and their parts derived from arterial oftalmika, the first major branch of the intracranial internal carotid artery. This branch runs below the optic nerve and optic canal with him through to the orbita. The first intraorbital branch is the central retinal artery, which enter the optic nerve about 8-15 mm behind the eyeball. Retinal blood vessels out in papil N. II, forming a picture of the different branches on each individual.
The retina receives blood from two sources. Usually the inside of the retina is supplied by central and branch a.retina memperdarahi inner two thirds. On the outside is supplied by koriokapiler which is right outside the Bruch membrane, which memperdarahi outer third of the retina. Includes outer layer pleksiformis and outer core layer, photoreceptors, and retinal pigment epithelial layer.
Senin, 21 Februari 2011
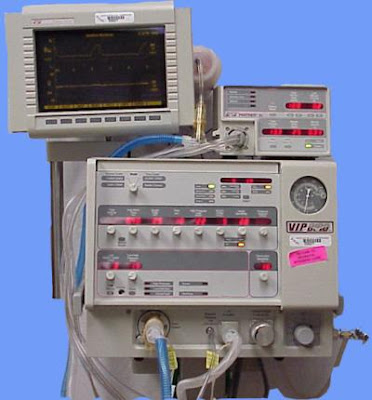
Microprocessor Usage on Ventilator
Pressure cycled Ventilator
1.Achieve Inspiration stops when pressure has been set previously, then the passive expiratory
2.Used mainly short-term tx <24 hours
3.Reduce / can cause barotrauma to the predetermined setpressure
4.Disadvantages: high in RAW & Complience bad lung maydecrease TV
5.There is no "Automatic Sigh" re expand the alveoli to preventatelektase
Volume cycled Ventilator
1.Most commonly used
2.Inspiration stops when the specified volume is reached
3.No matter the pressure is reached and then just happenedexpiratory
Time Cyceld Ventilator
1.inspiration to expiration based on time
2.tidal volume occurred from RR and MV
3.This is generally for neonatal ventilator
High Frequency Ventilator
1.Using the RR (usually 4x) high with a small TV (<death space) tokeep the alveoli to remain terventilasi, prevent barotraumas
2.Three variations on this type:
High frequency positive pressure ventilation
High frequency jet ventilation
High Frequency Oscillation
3.Purpose Mechanical Ventilation
4.Reduce Work Breathing (WOB)
5.Improve Patient Comfort Level
6.Providing accurate MV
7.Addressing imbalances V / P
8.Ensuring adequate kejaringan O2 delivery
Classification and Settings Ventilator
Ventilator Classification
1. Characteristics Inspiration
a. Constant Flow Generator
b. Non-constant Flow Generator
c. Constant Pressure Generator
2. Exchange Cycle Phase-Ekspirasi Inspiration
a. Time cycled ventilator
b. Volume cycled Ventilator
c. Pressure cycled Ventilator
3. Microprosessor-Controlled Ventilator
a. Machines can be modified / arranged according to the desired function
b. Microprosessor allowing ventilator settings tsb
Ventilator Settings
Depending on the type of respiratory failure, partial or total ventilation support
1. Total Ventilation Support: (CMV, AC, PCV) generally:
a. RR 10-12 x / min
b. TV 80-10 ml / kg to prevent: high PAW, Volu or Barotrauma
2. Partial Support Ventilation
a. Usually low SIMV <8 x / '
b. Tidal volume of 6-10 ml / kg, with or without PS
c. Patients breathing spontaneously with SIMV must overcome resistance from the ETT, valve, ventilator breathing circuit
d. ETT small (<7.0-7.5) should be avoided
e. The use of simultaneous SIMV PS 5-15 cmH2O to overcome resistance of the ETT & circuit
f. The addition of PS 5-8 cmH2O during positive ventilation and gas exchange to maintain PRC
Ventilator
Definition:
Ventilator is a device used to helped in part or whole process of ventilation to maintain oxygenation
Indications Ventilator Installation
Ventilator Mode:
Ventilator is a device used to helped in part or whole process of ventilation to maintain oxygenation
Indications Ventilator Installation
- Patients unable to breathe spontaneously
- Patients breathe but not enough to develop breast
- Resuscitation kardiopulmonar
- Failure of chronic and acute respiratory
- The use of general anesthesia
- Increase the excretion of carbon dioxide
- Failed kardiopulmonar
- Ventilator prophylaxis
Ventilator Mode:
- CONTROL MODE (CMV)
- ASSIST CONTROL MODE ventilator (ACMV)
- SYNCRONISED INTERMITENT mandatory ventilation (SIMV)
- SUPPORT pressure ventilation (PSV)
- Continues positive airway pressure (CPAP)
- POSITIVE END EKSPIRATORY pressure (PEEP)
Medicines Cardiovascular Support
Medicines Cardiovascular Support
1. Epineprin (adrenaline)
Very useful to overcome cardiac arrest in VT / VF without a pulse and because it has the effect asistole vasokontriktor.
Epineprin given at a dose of 1 mg in a bolus and then rinsed with NaCl ± 10-20 ml, 3-5 minutes of administration can be repeated. If IV not available to diberiakn melaului epineprin ETT with a dose of 2-2, 5 mg.
2. Atropine (SA)
SA serves to increase the frequency of pulse and increase blood pressure is recommended in asistole and PEA (HR: 60x/menit) with a dose of 1 mg can be repeated 3-5 minutes until maximum dose of 3 mg. melaluui given IV bolus and then rinsed with D5% or NaCl 0.9% ± 10-20 ml.
3. Norepineprin
Vasoconstriction and inotropic drug is strong. Norepineprin improve renal blood flow and urine output. Norepineprin can be effective in the management of patients with severe hypotension (systolic blood pressure <70 mmHg)
The initial dose is 0.5 to 1 μ norepineprin / ml was titrated until the visible effect
4. Adenosine
Adenosine can inhibit the activity of the SA node and AV, recommended indications:
4.1 Tachycardia SA or AV node reentry
4.2 SVT unstable during the preparation cardioversion
Preparation of 6 mg rapid IV bolus (1-3 seconds) bebarengan with 0.9% NaCl bolus of 20cc. If no change in cadence subs 1-2 minutes to give back 12 mg rapid bolus.
5. Amiodarone (Cordaron)
Amiodarone can cause vasodilation and hypotension that gift should be a slow infusion. The use of amiodarone is the treatment of life-threatening ventricular arrhythmias.
Provision of amiodarone of 150 mg for 10 minutes, followed by 1 mg per minute for 6 hours and 0.5 mg per minute subs 18 hours
6. Lidocain
1. Epineprin (adrenaline)
Very useful to overcome cardiac arrest in VT / VF without a pulse and because it has the effect asistole vasokontriktor.
Epineprin given at a dose of 1 mg in a bolus and then rinsed with NaCl ± 10-20 ml, 3-5 minutes of administration can be repeated. If IV not available to diberiakn melaului epineprin ETT with a dose of 2-2, 5 mg.
2. Atropine (SA)
SA serves to increase the frequency of pulse and increase blood pressure is recommended in asistole and PEA (HR: 60x/menit) with a dose of 1 mg can be repeated 3-5 minutes until maximum dose of 3 mg. melaluui given IV bolus and then rinsed with D5% or NaCl 0.9% ± 10-20 ml.
3. Norepineprin
Vasoconstriction and inotropic drug is strong. Norepineprin improve renal blood flow and urine output. Norepineprin can be effective in the management of patients with severe hypotension (systolic blood pressure <70 mmHg)
The initial dose is 0.5 to 1 μ norepineprin / ml was titrated until the visible effect
4. Adenosine
Adenosine can inhibit the activity of the SA node and AV, recommended indications:
4.1 Tachycardia SA or AV node reentry
4.2 SVT unstable during the preparation cardioversion
Preparation of 6 mg rapid IV bolus (1-3 seconds) bebarengan with 0.9% NaCl bolus of 20cc. If no change in cadence subs 1-2 minutes to give back 12 mg rapid bolus.
5. Amiodarone (Cordaron)
Amiodarone can cause vasodilation and hypotension that gift should be a slow infusion. The use of amiodarone is the treatment of life-threatening ventricular arrhythmias.
Provision of amiodarone of 150 mg for 10 minutes, followed by 1 mg per minute for 6 hours and 0.5 mg per minute subs 18 hours
6. Lidocain
Extubation
Definition: the removal of the tracheal tube ETT
Requirements:
1) Patients are aware or to cough effectively
2) stable vital signs and no hypoxia
3) sedative medications are minimal and not influenced by muscle relaxan
4) Tidal volume of patients over 5cc/kg
5) the underlying disease in patients for intubation improved
Objectives:
1) As the final stage and the process of weaning from ventilator
2) In order for the patient to breathe spontaneously
3) In order for the patient to cough effectively and can issue its own sputum
Procedure:
1. Preparation Equipment:
• Set full suction
• suction catheter
• O2 NRM
• Set intubation
• Gloves
• Spuit 20 ml
• Drugs and inhalation premediakasi physician orders
• Spirometry
• Emergency trolly
2. Implementation
a) Nurses wash their hands and wear gloves
b) Inform and explain if the patient is unconscious) regarding the actions taken
c) Monitor vital signs (stable)
d) Patients fasted
e) Check AGD
f) Check the tidal volume by spirometry
g) NGT flowed with plastic bags
h) Give pre-medication drugs as directed, onat inhalation, adrenaline + NaCl 0.9% or Ventolin and pulmicort, such as the type of corticosteroid injection drug
i) Perform suction mucus through the mouth and clean ETT
j) Cuff dikempeskan
k) ETT fixation patch released
l) Time of appointment ETT, suction hose must exist in the ETT to suck mucus until the ETT in drag
m) Perform suction through the mouth
n) Install the NRM 10 lpm O2
o) Position the patient semi-Fowler and give appropriate instructions inhalation therapy
p) Tidy tool
q) The nurse took off the gloves and wash hands
r) Observation of vital signs and 1 hour and then re-check AGD
Requirements:
1) Patients are aware or to cough effectively
2) stable vital signs and no hypoxia
3) sedative medications are minimal and not influenced by muscle relaxan
4) Tidal volume of patients over 5cc/kg
5) the underlying disease in patients for intubation improved
Objectives:
1) As the final stage and the process of weaning from ventilator
2) In order for the patient to breathe spontaneously
3) In order for the patient to cough effectively and can issue its own sputum
Procedure:
1. Preparation Equipment:
• Set full suction
• suction catheter
• O2 NRM
• Set intubation
• Gloves
• Spuit 20 ml
• Drugs and inhalation premediakasi physician orders
• Spirometry
• Emergency trolly
2. Implementation
a) Nurses wash their hands and wear gloves
b) Inform and explain if the patient is unconscious) regarding the actions taken
c) Monitor vital signs (stable)
d) Patients fasted
e) Check AGD
f) Check the tidal volume by spirometry
g) NGT flowed with plastic bags
h) Give pre-medication drugs as directed, onat inhalation, adrenaline + NaCl 0.9% or Ventolin and pulmicort, such as the type of corticosteroid injection drug
i) Perform suction mucus through the mouth and clean ETT
j) Cuff dikempeskan
k) ETT fixation patch released
l) Time of appointment ETT, suction hose must exist in the ETT to suck mucus until the ETT in drag
m) Perform suction through the mouth
n) Install the NRM 10 lpm O2
o) Position the patient semi-Fowler and give appropriate instructions inhalation therapy
p) Tidy tool
q) The nurse took off the gloves and wash hands
r) Observation of vital signs and 1 hour and then re-check AGD
LMA (laryngeal mask airway)
Indications: if found difficulty in endotracheal intubation time
The installation procedure:
The installation procedure:
- Empty the cuff and do not have folds in the mask
- Give him pelican or jelly
- The bowl of the cuff facing thethe front of the of the mouth,press into the soft palate and pharyngeal wall .
- Enter the cuff into the hypopharynx until resistance is felt
- Inflate cuff
- Do baging, consider the development of the chest when there are air leaks, fix the position of LMA, remove and re-enter.
Pipe Fitting endotracheal tube (Pet) or intubation
Intubation is the act of maintaining the airway by inserting the pipe through the mouth and nose into the trachea.
ETT installation Benefits:
PROCEDURE
1. Preparation Equipment:
2. Implementation
Complications of intubation Actions
ETT installation Benefits:
- Maintenance of airway
- Ensure the provision of oxygen
- Prevent aspiration
- Facilitate the exploitation of mucus or sputum in the trachea.
- Driveway is some kind of resuscitation medicine.
PROCEDURE
1. Preparation Equipment:
- - Laryngoscope with blades in accordance with needs
- - Margil forceps to help insert pipe ETT
- - Mandrain or stylet for ETT curvature memanipulsi
- - ETT as needed psien
- - Cylocain jelly
- - Cylocain spray
- - Cup kidney and duk (sterile)
- - Gloves
- - Drugs in preparation for intubation include sedation (Diprivan, dormicum, relaxan, MO, norcuron)
- - Cuff inflator
- - Spuit 20 ml
- - Gudel or mayo tube
- - Stethoscope
- - Suction Catheter
- - Set suction
- - Ambubag + lid
- - Hipafix
- - Scissors
- - Suction wall
- - Thin Pillow
2. Implementation
- a) Inform and explain (if the patient is conscious) actions to be performed on patients and families
- b) Prepare a letter of approval actions to be signed
- c) Nurses wash their hands and wear gloves
- d) Check kepatenan ETT cuff with 20 ml syringe
- e) Put down the sterile cup placed thereon and then apply a sterile kidney Xilocain jelly on the surface of the ETT tip and put mandarin and forcep margil already didesinfektan with alcohol
- f) Check and adjust the central suction pressure between 100-200 mmHg and plug it into a sterile suction catheter.
- g) Clean the airway mucus by suction (if necessary use mayo)
- h) Set the position of the patient in a supine position, head ekstensikan
- i) Assist appropriate action intuasi SPO (including the provision of sedation according to doctor's instructions)
- j) If successful banging then auscultation in the epigastrium, right and left chest (up-down)
- k) If the entry is correct ETT position recharge cuff with syringe
- l) ETT fixation with plaster, hipafix according to the depth limit
- m) Connect the ETT with oxygen / ventilator required
- n) Note the patient's general condition, during and after the act of intubation
- o) Measure pressure cuff with cuff pressure (20-30 mmHg)
- p) Take the culture if necessary
- q) Tidy tool
- r) Contact officer for inspection photos radiology thorax
Complications of intubation Actions
- Injury to the lips and tongue due to pinched laryngoscope
- Tooth fracture
- laceration of the pharynx and trachea due Stilets / mandarin and ETT tip
- Damage to vocal cords
- Vomiting and aspiration
- The liberation of adrenaline and noradrenaline intubation due to stimulation resulting in hypertension, and arrhythmias tachikardi
Equipment For Emergency Situation
The first time people experience gravity conditions, the nurse will call someone to come give relief assistance and began providing basic life support, the other team immediately took emergency trolly and defibrillators to near in addition to the patient.
Trolly emergency in the preparation is very varied but basically consist of basic emergency equipment and medicines. Health workers must understand and know where to store emergency trolly. Trolly emergency is as a storage device consisting of a closed storage and some drawers. The order of storage of equipment in each type of emergency trolly.
Trolly emergency in the preparation is very varied but basically consist of basic emergency equipment and medicines. Health workers must understand and know where to store emergency trolly. Trolly emergency is as a storage device consisting of a closed storage and some drawers. The order of storage of equipment in each type of emergency trolly.
- Resuscitation board usually located in the rear / side. Board was later placed under the patient's back as a hard base when performed chest compression.
- Monitor / defibrillator was placed at the top of trolly. Patients with heart rhythm disturbances in the monitor via leads and electrodes on the machine. When used in defibrillation placed on the chest that is used in a rapid, this method is used to restore heart rhythm to normal direction.
- A transcutaneous pacemaker is placed on a trolly emergency or some parts of the monitor or defibrillator units.
- Bagging and containment oxygen mask and tubing is usually placed above the ET. Oxygen hose connected to a central oxygen or a wall or portable oxygen.
- Equipment to maintain the airway, such as mayo bias placed in one box (the drawer emergency trolly).
- Another drawer contains a fluid infusion. Infuse the form of: NaCl, RL, colloid, dextrose 5% which is also used to supply.
- The contents of the next drawer contains emergency drugs are needed, which is usually given by injection or drip like adrenaline, SA, lidocain, dopamine, vascon, etc..
- Another drawer contains a suction catheter, NGT, albocath, needles, infusion sets, etc..
- Trolly this should be checked every shift every 24 hours to determine the completeness of equipment and whether the equipment functioning optimally.
- Every nurse should know and understand where storage locations, the nurse should take turns to be responsible for the completeness of emergency trolly.
Trolley Emergency
Each health workers especially nurses in hospitals to understand and know about basic life support and advanced life support. Basic life support includes assessment of symptoms and signs of sudden cardiac arrest, heart attack, stroke and airway obstruction by foreign body, with cardiac pulmonary resuscitation (CPR) and automated external defibrillators defribilasi with (AED).
There are 4 pieces of the circle in a floor (the "Chain of Survival") to illustrate the action helper with sudden cardiac arrest with ventricular fibrillation / asphyxia. When stroke patients arrive at hospital emergency room, initial treatment should be started within 10 minutes, the CT scan must be done within 25 minutes and fibrolitik therapy was started within 60 minutes after arriving in the emergency room and within 3 hours of onset of symptoms.
The Chain Of Survival consists of:
1. Early Access
Quickly identify objec emergency and activate the emergency system (by calling someone untukmenolong)
2. Early CPR
Quickly perform CPR (CPR continue to be done until other rescuers arrived)
3. Early Defibrilation
Quickly perform defibrillation, CPR with defibrillation within 3-5 minutes early, can increase the success rate between 49% - 75%.
4. Early ACLS
Sooner done advanced life support followed by post-resuscitation aid.
There are 4 pieces of the circle in a floor (the "Chain of Survival") to illustrate the action helper with sudden cardiac arrest with ventricular fibrillation / asphyxia. When stroke patients arrive at hospital emergency room, initial treatment should be started within 10 minutes, the CT scan must be done within 25 minutes and fibrolitik therapy was started within 60 minutes after arriving in the emergency room and within 3 hours of onset of symptoms.
The Chain Of Survival consists of:
1. Early Access
Quickly identify objec emergency and activate the emergency system (by calling someone untukmenolong)
2. Early CPR
Quickly perform CPR (CPR continue to be done until other rescuers arrived)
3. Early Defibrilation
Quickly perform defibrillation, CPR with defibrillation within 3-5 minutes early, can increase the success rate between 49% - 75%.
4. Early ACLS
Sooner done advanced life support followed by post-resuscitation aid.
Effects On Ventilation And oxygenation
Effects On Ventilation And oxygenation
1. Work breath will increase in the state of increased airway resistance
- This will cause adverse effects on ventilation and oxygenation
2. Failed ventilation decreased minute ventilation of patients (TV x RR) and is unable to remove the CO2 production
3. Failed oxygenation occurs during the respiratory system is unable to provide adequate oxygen required for metabolism
1. Work breath will increase in the state of increased airway resistance
- This will cause adverse effects on ventilation and oxygenation
2. Failed ventilation decreased minute ventilation of patients (TV x RR) and is unable to remove the CO2 production
3. Failed oxygenation occurs during the respiratory system is unable to provide adequate oxygen required for metabolism
RAW And Work Of Breathing
Airway Resistance (RAW) And Work Of Breathing
A. Airway resistance is calculated based on the change in pressure / flow of air = pressure change / Flow
B. Raw = (P2 - P1) / flow
1. P2 = Peak airway pressure
2. P1 = Plateau pressure
3. Flow = liters / sec
C. Any increase in airway resistance would improve the work of breath
D. Patients who are unable to overcome resistance by increasing the road winded breath work
E. In patients with chronic astma (chronic airway obstruction), there was water traping so high lung compliance, and therefore the pattern of breath but usually in the slowly
- However, in patients with COPD (lung restriktive) pattern is fast and shallow breathing, because the cause is not obstruction
A. Airway resistance is calculated based on the change in pressure / flow of air = pressure change / Flow
B. Raw = (P2 - P1) / flow
1. P2 = Peak airway pressure
2. P1 = Plateau pressure
3. Flow = liters / sec
C. Any increase in airway resistance would improve the work of breath
D. Patients who are unable to overcome resistance by increasing the road winded breath work
E. In patients with chronic astma (chronic airway obstruction), there was water traping so high lung compliance, and therefore the pattern of breath but usually in the slowly
- However, in patients with COPD (lung restriktive) pattern is fast and shallow breathing, because the cause is not obstruction
Minggu, 20 Februari 2011
Airway Resistance
DEFINITION:
-Blockage (obstruction) of air in the airway
-On mechanical ventilation, the degree of weight resistance mainly influenced by the size (diameter), length and airway patency, length of endotracheal tube and circuit
Factors affecting the airway resistance:
A. Resistance increases if the airway diameter decreases
B. Obstruction to airflow can be caused by changes in:
1. In the airway (sputum retention)
2. In the airway wall (tumor on the bronchial muscle structure)
3. Outside the airway (tumors that surround and suppress airway)
4. When these factors occur, the airway diameter will shrink so that the increased airway resistance
5. So if the airway diameter is reduced ½ of the normal, then the pressure required to incorporate as much air flow as normal time will increase 16 times
C. Of the few diseases that can increase airway resistance, COPD is the commonest
1. This type includes emphysema, chronic bronchitis, chronic asthma, and bronkletasis
2. Mechanical conditions that may also increase airway resistance is obstruction post-intubation and aspiration of foreign bodies
3. The process of infection include laringotrakeobronkitis, epiglottitis and bronchiolitis
D. Normal airway resistance ranged between 0.6 and 2.4 cmH20/liter/detik can stream flow (air flow) of 38 liters / minute (0.5 liters / sec)
1. Will increase the terintubasi apasien pad, and depending on the size of ETT
2. Airway resistance will change at any time and directly proportional to the length of ETT and inversely proportional to the diameter of the ETT
3. For that ETT is a good measure of the largest ETT according to patient's trachea
4. Nukus plaq in ETT was instrumental in increasing airway resistance
E. Ventilator Circuit also affect resistance to airflow from the ventilator, or play a role in increasing airway resistance
F. The important thing also is the amount of water (water), condensation in the ventilator circuit, if the number will increase quite a lot of resistance also
-Blockage (obstruction) of air in the airway
-On mechanical ventilation, the degree of weight resistance mainly influenced by the size (diameter), length and airway patency, length of endotracheal tube and circuit
Factors affecting the airway resistance:
A. Resistance increases if the airway diameter decreases
B. Obstruction to airflow can be caused by changes in:
1. In the airway (sputum retention)
2. In the airway wall (tumor on the bronchial muscle structure)
3. Outside the airway (tumors that surround and suppress airway)
4. When these factors occur, the airway diameter will shrink so that the increased airway resistance
5. So if the airway diameter is reduced ½ of the normal, then the pressure required to incorporate as much air flow as normal time will increase 16 times
C. Of the few diseases that can increase airway resistance, COPD is the commonest
1. This type includes emphysema, chronic bronchitis, chronic asthma, and bronkletasis
2. Mechanical conditions that may also increase airway resistance is obstruction post-intubation and aspiration of foreign bodies
3. The process of infection include laringotrakeobronkitis, epiglottitis and bronchiolitis
D. Normal airway resistance ranged between 0.6 and 2.4 cmH20/liter/detik can stream flow (air flow) of 38 liters / minute (0.5 liters / sec)
1. Will increase the terintubasi apasien pad, and depending on the size of ETT
2. Airway resistance will change at any time and directly proportional to the length of ETT and inversely proportional to the diameter of the ETT
3. For that ETT is a good measure of the largest ETT according to patient's trachea
4. Nukus plaq in ETT was instrumental in increasing airway resistance
E. Ventilator Circuit also affect resistance to airflow from the ventilator, or play a role in increasing airway resistance
F. The important thing also is the amount of water (water), condensation in the ventilator circuit, if the number will increase quite a lot of resistance also
Sabtu, 19 Februari 2011
System On Ventilator
Alarm System
1. Ventilators are used to support life
2. Alarm systems need to alert nurses
about a problem
3. Low pressure alarm indicates the termination
of patients (regardless of the patient's ventilator)
4. Indicate a high pressure alarm
increased pressure, eg patients with cough, tubing
bent, there is fighting, etc.
5. Low volume indicates a leak alarm
6. Alarms should never be ignored and not considered
shall be installed in a condition ready
Humidifikasi and Temperature System
1. All the air that flowed from the ventilator
through the water in the humidifier warmed and saturated
2. The temperature is set approximately equal to the temperature
body
3. In cases of severe hipotermi, air conditioning
can be improved
4. Temperatures that are too high can cause injury
fuel in the trachea
5. When the temperature is too low can lead to
drought airway and secretions become thick
so hard to do the exploitation
1. Ventilators are used to support life
2. Alarm systems need to alert nurses
about a problem
3. Low pressure alarm indicates the termination
of patients (regardless of the patient's ventilator)
4. Indicate a high pressure alarm
increased pressure, eg patients with cough, tubing
bent, there is fighting, etc.
5. Low volume indicates a leak alarm
6. Alarms should never be ignored and not considered
shall be installed in a condition ready
Humidifikasi and Temperature System
1. All the air that flowed from the ventilator
through the water in the humidifier warmed and saturated
2. The temperature is set approximately equal to the temperature
body
3. In cases of severe hipotermi, air conditioning
can be improved
4. Temperatures that are too high can cause injury
fuel in the trachea
5. When the temperature is too low can lead to
drought airway and secretions become thick
so hard to do the exploitation
Jumat, 18 Februari 2011
Lid CPAP (Cuntinuous positive airway pressure)
Lid CPAP (Cuntinuous positive airway pressure)
- Provide a positive pressure into the airway to open the alveoli, improving functional residual capacity, and improve oksigeneration
- is indicated for patients breathing spontaneously with an experienced hiposekmia due to atelectasis
ADVANTAGES:
Provide positive pressure ventilator without installation
ADVANTAGES:
- The possibility of vomiting with aspiration, which can be prevented by way of gastric decompression
- Not convenient for patients, erythema, skin abrasions around the depressed area (nose, cheeks, chin)
- Decrease in cardiac output and hypotension because of positive pressure in the thoracic
Ventury Mask
VENTURY MASK
- Provide flow that varies with the concentration of 24-60%
- Forms such as containment, but he has a jet adapter between the lid and tubing to the source oksigen.Jet adapter consists of varying sizes (often marked by color) that shows the value of FIO2.
Table Instructions Ventury color mask
ADVANTAGES:
- To provide the desired concentration of O2
- Work for the patients when given excessive oxygen can mendepresi respiratory drive
LOSSES:
- Limitations of the patient to eat, drink, and cough
- May cause irritation to the eyes because the flow meter, for high concentrations use a humidifier
- Set flow meter as stated on the lid
- Adjust the straps so that the lid close lid tightly and comfortably, if necessary, use a gauze in a depressed area
- Provide flow that varies with the concentration of 24-60%
- Forms such as containment, but he has a jet adapter between the lid and tubing to the source oksigen.Jet adapter consists of varying sizes (often marked by color) that shows the value of FIO2.
Table Instructions Ventury color mask
ADVANTAGES:
- To provide the desired concentration of O2
- Work for the patients when given excessive oxygen can mendepresi respiratory drive
LOSSES:
- Limitations of the patient to eat, drink, and cough
- May cause irritation to the eyes because the flow meter, for high concentrations use a humidifier
- Set flow meter as stated on the lid
- Adjust the straps so that the lid close lid tightly and comfortably, if necessary, use a gauze in a depressed area
Lid Non-Rebreathing
Lid Non-Rebreathing
- Provides O2 with a flow of 6-12 L / min with 80-100% O2 concentration
- The design looks like the face shield with a rebreathing bag, but the lid has a unidirectional valve between the reservoir bag and the lid on the hole in the side of the lid ekshalasi
- The purpose of the valve is to prevent ekshalasi air into the bag and prevent entry of room air. At the moment of inspiration, the valve on the side of the valve closes and the connection between the bag and the lid is opened, allowing 100% O2 inhalation. At the time of expiration, the valve opens and the side of the valve between the bag and close the lid, increase the release of ekshalasi air out and prevent the entry into the bag.
- The air does not mix inspiration with expiratory air
ADVANTAGES:
O2 Gives 80% for patients with severe hiposekmia
LOSSES:
- Not convenient for patients
- Limitations to eat, drink, cough
- The possibility of inherent valve
- Irritation of the eyes due to high O2 flow rate and the lid that does not fit on the nose
How to Install
- Explain the procedure in patients
- Connect the hose O2 on the humidifier with low flow
- The contents of O2 into the bag by closing the hole between the pouch with a lid
- Adjust the straps tightly closed lid seghingga face and comfortable, if necessary, use a gauze in a depressed area
- Adjust the flow of O2 so that the bag will be filled when the expression and nearly bud at the time of inspiration.
- Provides O2 with a flow of 6-12 L / min with 80-100% O2 concentration
- The design looks like the face shield with a rebreathing bag, but the lid has a unidirectional valve between the reservoir bag and the lid on the hole in the side of the lid ekshalasi
- The purpose of the valve is to prevent ekshalasi air into the bag and prevent entry of room air. At the moment of inspiration, the valve on the side of the valve closes and the connection between the bag and the lid is opened, allowing 100% O2 inhalation. At the time of expiration, the valve opens and the side of the valve between the bag and close the lid, increase the release of ekshalasi air out and prevent the entry into the bag.
- The air does not mix inspiration with expiratory air
ADVANTAGES:
O2 Gives 80% for patients with severe hiposekmia
LOSSES:
- Not convenient for patients
- Limitations to eat, drink, cough
- The possibility of inherent valve
- Irritation of the eyes due to high O2 flow rate and the lid that does not fit on the nose
How to Install
- Explain the procedure in patients
- Connect the hose O2 on the humidifier with low flow
- The contents of O2 into the bag by closing the hole between the pouch with a lid
- Adjust the straps tightly closed lid seghingga face and comfortable, if necessary, use a gauze in a depressed area
- Adjust the flow of O2 so that the bag will be filled when the expression and nearly bud at the time of inspiration.
Hospital Characteristics
Hospital organizations have some properties that do not simultaneously possess other organizations in general. Nature or other characteristics are:
* As of hospital workers are professionals
* The authority's head is different from the hospital authority employers.
* The duties of a professional group more than the managerial group work
* Work expenses can not be ruled
* The number of jobs and nature of work in diverse work units
* Almost all activities are urgent
* Services are very individualistic sifatya hospital
* The task to provide the service is personal. These services must be fast and accurate, errors can not be tolerated
* Service runs continuously 24 in a day
As a result of the ongoing nature of the service are:
* The requirement of power supply that is always ready at any time
* The requirement of equipment that is always ready, the electricity that should not be stopped
* Monitoring ongoing
* Must be always available operational funds at any time
* The service is emergency, should be done immediately
State of emergency nature should get service immediately, because they can not be delayed by issues related to the life-death patients
* Negligence, carelessness for the services can not be tolerated
* Modern hospital is an institution with solid technology, many using advanced tools
* Educational background of the diverse demands ruamh pain awareness to create a good cooperation
* Services hospital became the focus of attention and control of society.
* Another characteristic that marks the uniqueness of the hospital is a building, where mamberikan service is a building designed in such a way that meets the requirements or standards yag determined.
* As of hospital workers are professionals
* The authority's head is different from the hospital authority employers.
* The duties of a professional group more than the managerial group work
* Work expenses can not be ruled
* The number of jobs and nature of work in diverse work units
* Almost all activities are urgent
* Services are very individualistic sifatya hospital
* The task to provide the service is personal. These services must be fast and accurate, errors can not be tolerated
* Service runs continuously 24 in a day
As a result of the ongoing nature of the service are:
* The requirement of power supply that is always ready at any time
* The requirement of equipment that is always ready, the electricity that should not be stopped
* Monitoring ongoing
* Must be always available operational funds at any time
* The service is emergency, should be done immediately
State of emergency nature should get service immediately, because they can not be delayed by issues related to the life-death patients
* Negligence, carelessness for the services can not be tolerated
* Modern hospital is an institution with solid technology, many using advanced tools
* Educational background of the diverse demands ruamh pain awareness to create a good cooperation
* Services hospital became the focus of attention and control of society.
* Another characteristic that marks the uniqueness of the hospital is a building, where mamberikan service is a building designed in such a way that meets the requirements or standards yag determined.
LID REBREATHING
INTERFACE WITH BAG LID REBREATHING
- Provide O2 with a flow of 8-12 L / min with a concentration of 40-60%
- Design rebreathing face shield similar to a simple face shield, with the addition of O2 reservoir bag
-Air inspiration partly mixed with air expression, 1 / 3 part ekshalasi volume into the bag, 2 / 3 part ekshalasi volume through the holes on the side
ADVANTAGES:
Saving Oxygen ekshalasi of anatomic dead space
LOSSES:
- Flow rate is not fit to lead back to CO2 inhalation
- Patients are not free to eat, drink, or cough
DANGER:
- There was an aspiration if vomiting
- Emphysema subcutaneous tissue into the eye at high O2 flow
- Necrosis due to mounting face that is too tight lid
MAINTENANCE:
- Advance the patient is cleaned and dried every 2 hours
- Fume face replaced / cleaned every 8 hours
- If there is water in the bag, it must be emptied
How to Install
- Explain the procedure in patients
- Connect the hose O2 on humidifier with low flow
- The contents of O2 into the bag by closing the hole between the pouch with a lid
- Adjust straps so that the lid closes tightly and comfortably, if necessary, wear gauze pads in a depressed area
- Adjust the flow of O2 so that the bag will be filled in expiratory time and inspiration time nearly bud
- Provide O2 with a flow of 8-12 L / min with a concentration of 40-60%
- Design rebreathing face shield similar to a simple face shield, with the addition of O2 reservoir bag
-Air inspiration partly mixed with air expression, 1 / 3 part ekshalasi volume into the bag, 2 / 3 part ekshalasi volume through the holes on the side
ADVANTAGES:
Saving Oxygen ekshalasi of anatomic dead space
LOSSES:
- Flow rate is not fit to lead back to CO2 inhalation
- Patients are not free to eat, drink, or cough
DANGER:
- There was an aspiration if vomiting
- Emphysema subcutaneous tissue into the eye at high O2 flow
- Necrosis due to mounting face that is too tight lid
MAINTENANCE:
- Advance the patient is cleaned and dried every 2 hours
- Fume face replaced / cleaned every 8 hours
- If there is water in the bag, it must be emptied
How to Install
- Explain the procedure in patients
- Connect the hose O2 on humidifier with low flow
- The contents of O2 into the bag by closing the hole between the pouch with a lid
- Adjust straps so that the lid closes tightly and comfortably, if necessary, wear gauze pads in a depressed area
- Adjust the flow of O2 so that the bag will be filled in expiratory time and inspiration time nearly bud
Simple Home Lid
Simple Home Lid
- Provides O2 with a flow of 5-8 L / min
- It has a ventilation hole in the side kesua to the entry of room air and air discharge of expression, has no valve or reservoir bag
ADVANTAGES:
- Simple, light weight
- Provides up to 60% FIO2
LOSSES:
- Patients are not free to speak, eat, drink
- Can cause dryness and irritation to eyes
- If the patient is attached NGT, it is difficult for the correct application
DANGER:
- There was an aspiration if vomiting
- Stacking CO2 at low flow
- Emphysema subcutaneous tissue into the eye at high O2 flow
- necrosis if the face is set too tight lid
MAINTENANCE:
In intermittent, clean the inside of the mask and dry sir that accumulate around the mask. Assess the depressed area of skin
How to Install
- Explain the procedure to be performed on patients
- Connect the hose to the humidifier O2 with low O2 flow
- Adjust the straps so that the lid close lid tightly and comfortably, if necessary, wear pads on the depressed area
- Provides O2 with a flow of 5-8 L / min
- It has a ventilation hole in the side kesua to the entry of room air and air discharge of expression, has no valve or reservoir bag
ADVANTAGES:
- Simple, light weight
- Provides up to 60% FIO2
LOSSES:
- Patients are not free to speak, eat, drink
- Can cause dryness and irritation to eyes
- If the patient is attached NGT, it is difficult for the correct application
DANGER:
- There was an aspiration if vomiting
- Stacking CO2 at low flow
- Emphysema subcutaneous tissue into the eye at high O2 flow
- necrosis if the face is set too tight lid
MAINTENANCE:
In intermittent, clean the inside of the mask and dry sir that accumulate around the mask. Assess the depressed area of skin
How to Install
- Explain the procedure to be performed on patients
- Connect the hose to the humidifier O2 with low O2 flow
- Adjust the straps so that the lid close lid tightly and comfortably, if necessary, wear pads on the depressed area
Cannula Binasal
Provides O2 with a concentration of 24-44% with flow 1-6L/menit.
Made from green or white plastic with a light weight, there are 2 Porong inserted into the patient's nose
ADVANTAGES:
- Patients can move freely, eat, drink and talk
- Efficiency and comfort for patients
- Can be used for patients with COPD
- Cheap
- Hose easily adapted to the patient's face
LOSSES:
- May cause irritation to the nose, the back of the ears where the rope binasal
- The concentration of oxygen is reduced when the patient breathes through the mouth
DANGER:
Nasal irritation, drying of the nasal mucosa, sinus pain and epitaksis
MAINTENANCE:
Check each time the location of the tip of the nose cannula and observation of obstruction
How to Install
- Explain the procedure in patients
- Connect the cannula to the oxygen hose to the humidifier with low oxygen flow. Insert both ends of the cannula into the nostrils
- Fixation oxygen hose
Made from green or white plastic with a light weight, there are 2 Porong inserted into the patient's nose
ADVANTAGES:
- Patients can move freely, eat, drink and talk
- Efficiency and comfort for patients
- Can be used for patients with COPD
- Cheap
- Hose easily adapted to the patient's face
LOSSES:
- May cause irritation to the nose, the back of the ears where the rope binasal
- The concentration of oxygen is reduced when the patient breathes through the mouth
DANGER:
Nasal irritation, drying of the nasal mucosa, sinus pain and epitaksis
MAINTENANCE:
Check each time the location of the tip of the nose cannula and observation of obstruction
How to Install
- Explain the procedure in patients
- Connect the cannula to the oxygen hose to the humidifier with low oxygen flow. Insert both ends of the cannula into the nostrils
- Fixation oxygen hose
Nasal Catheter
Provides O2 with flow 1-3 L / min with a concentration of 24-32%. Made of plastic or rubber with about 39 cm long with 6-8 hole at the tip of the catheter. The depth of the catheter from the nasal side of the pharynx was measured by measuring the distance from ears to nose
ADVANTAGES:
- Provision of stable O2
- Patients are free to move, talk, eat or drink
LOSSES:
- Can occur nasopharyngeal mucous membrane irritation
- The catheter is easily clogged with secretions or bent
- Inserting a catheter technique is rather difficult
- Unable to provide more than 40% concentration
DANGER:
Drying the nasal mucosa, the possibility of gastric distension, epistaxis
Maintenance:
The catheter is changed every 8 hours and included kelubang another nose if possible. Fill humidifier with aquades height limit indicated on the bottle, do not be left blank
How to Install
- Explain the procedure in patients
-To estimate inside the catheter, measure the distance between the nostrils to the tip of the leaf ears
- Give lubricant (jelly) on the catheter tip
- Connect the catheter through the patent nostril as far as expected
- If the catheter tip is seen behind the uvula, pull the catheter so be on the verge of defeat is not visible anymore
- Use a plaster for fixation catheter
- After the patient is determined to move his head freely, then the tubes were fixed on the bed sheet
- Stream Oxygen in accordance with the needs of patients
ADVANTAGES:
- Provision of stable O2
- Patients are free to move, talk, eat or drink
LOSSES:
- Can occur nasopharyngeal mucous membrane irritation
- The catheter is easily clogged with secretions or bent
- Inserting a catheter technique is rather difficult
- Unable to provide more than 40% concentration
DANGER:
Drying the nasal mucosa, the possibility of gastric distension, epistaxis
Maintenance:
The catheter is changed every 8 hours and included kelubang another nose if possible. Fill humidifier with aquades height limit indicated on the bottle, do not be left blank
How to Install
- Explain the procedure in patients
-To estimate inside the catheter, measure the distance between the nostrils to the tip of the leaf ears
- Give lubricant (jelly) on the catheter tip
- Connect the catheter through the patent nostril as far as expected
- If the catheter tip is seen behind the uvula, pull the catheter so be on the verge of defeat is not visible anymore
- Use a plaster for fixation catheter
- After the patient is determined to move his head freely, then the tubes were fixed on the bed sheet
- Stream Oxygen in accordance with the needs of patients
OXYGEN THERAPY
Definition:
Oxygen therapy is to provide a flow of gas over 20% at a pressure of 1 atmosphere so that oxygen concentration increases in the blood to meet the needs of the body
Indications Giving Oxygen
1. Hypoxia, dyspnea, takipnes, disorientation, anxiety, apathy or decreased consciousness, tachycardia / bradycardia with blood pressure down.
2. Perioperative period, severe anemia
3. Airway obstruction
Objectives Provision of Oxygen
1. Increasing the amount of oxygen / oxygen pressure in alveoli
2. Reduced lung work
3. Reducing heart work
Method of Giving Oxygen
SYSTEM LOW FLOW
Provide O2 concentration that varies depending on the patient's breathing pattern
1. Concentration LOW LOW FLOW
- Nasal Catheter
- cannula binasal
2. Concentration HIGH LOW FLOW
- Fume simple face
- Fume face with Rebreathing bag
- Fume face with a bag Nonrebreathing
HIGH FLOW SYSTEM
Providing persistent O2 concentration
1. HIGH LOW FLOW Concentration
- Fume Ventury
2. HIGH FLOW HIGH Concentration
- Head Boxes
- Fume CPAP
Kamis, 17 Februari 2011
Thrombolytic
(Giving Streptase 1.5 million units)
Chest paint IMA > 20 ', retrosternal middle / left chest, radiating to jaw, back, left arm sepereti depressed heavy objects, crumpled like burning or tingling, can be pain in the epigastrium, cold sweat, nausea, vomiting, weakness , dizziness, floating, unconscious
WHO criteria for AMI
- Chest pain typical
- Evaluation of ECG
- There was an increase and then decrease in cardiac enzymes
- Hyperacute T, ST evaluation, T-inverted
ST evaluation of at least 0.1 mm in 2 contiguous sandapan
- BBB newly considered IMA
- Old infarction: QR V1 - V2> 0.035
Q I, II, aVL, aVF, V4 - V6 at least 1 mm
- Inferior infarction, suspected myocardial post 'N right ventricle
Check V3R - V4R and V7 - V9
Indications Streptase
- Acute myocardial infarct (no more than 12 hours) with ST evaluation or LBBB
- DVT (no more than 14 days)
- Acute massive pulmonary embolism
- Chronic arterial blockage (no more than 6 weeks)
- Acute and subacut thrombosis of peripheral arteries
Streptase 1.5 million can not be used for having an allergic reaction to the product caused the risk of bleeding during therapy given streptase 1.5 million so it can not be given in the conditions:
- Active internal bleeding (2-4 last week)
- Hemorrhagic stroke
- Bleeding intracranial or intraspinal (spinal cord surgery)
- Intracranial tumors
- Trauma to the head, a new trauma within 2-4 weeks
- Aneurysm
- Neoplasm with the risk of bleeding
- Acute pancreatitis
- Hypertension with systolic pressure over 200 mmHg and or diastolic pressure over 100 mmHg
- In the treatment of oral anticoagulation (INR> 1.3)
- Acute liver disease or kidney disease
- Endocarditis, or pericarditis
- Post major surgery (less than 3 weeks)
- The use of streptokinase (<2 years)
- History streptokinase allergy
- Pregnant
- Gastritis
Investigations
- Check CKMB started 4-8 hours
- Check triponin from 4-8 hours to 14 days repeated 12-24 hours later
Giving
1. Put IVline with venflon no. 20
2. Before the injection is given streptase given anti-allergy: dexametasone inj
3. Streptase 1.5 million units given intravenously, is given when BP> 100 mm Hg in 100 cc DS% / NaCl 0.9% finished in 1 hour
4. During the granting watch KU, tension, pulse, ECG, arrhythmias, bleeding and allergy patient complaints
5. Observations in every 5 minutes during the administration streptase
6. When the tension down, loading the Nacl, observation and pulse tension
7. Prepare medications such as dopamine, vascon and defibrillators
8. Observations EKG rhythm: VT, SVT
9. After 1 hour administration streptase carried out repeated ECG
10. Check CKMB enzyme, triponin I, AST / LDL 1 h post streptase
11. After 6 hours given heparin 5000 iu bolus followed 100 units / hour
12. 1 hour after administration of heparin, check APTI target of 1 ½ - 2 times the control
BASIC CAUSES OF DISEASE
A. Definition
1. The disease is the failure of the mechanism of adaptation of organisms to respond appropriately to stimuli or pressures causing interference with the function / structure of the organization or system of the body (Gold Medical Dictionary)
2. Disease is a condition in which the life process are no longer regular or interrupted his journey (Van Dale's Woordenboek der Nederlandse Tell)
Azwar (1988) concluded that the disease is:
A situation where there is disruption of form and function that are in a state that is not normal.
B. Development of Disease Occurrence Theory
At first, the concept is based on the existence of supernatural beings or interruption because of the wrath of the mighty creator.
The development of the theory of the next occurrence of the disease are:
1. Theory Contangion
The occurrence of disease is required contact between one person to another.
2. The theory of Hippocrates
Diseases caused by environmental influences in particular: water, air, soil, weather.
3. Humoral theory
Diseases caused by disorders of fluid balance in the human body.
4. Miasma Theory
Diseases caused by the remnants of living beings who experience decay, thus leaving air pollution and environmental
5. Epidemic Theory
Linking the occurrence of disease with weather and geographic (place)
6. The theory of micro-organism (germ terori)
Germs are considered as a single disease.
7. Nutrition and Resistance Theory
The observation of various epidemiological observations.
8. Environmental Ecology Theory
Humans interact with a variety of factors in certain circumstances and in certain circumstances would cause a specific disease.
C. Cause Compound
The disease has more than one cause, not a single character.
Causative factors are grouped into 4 groups, namely:
1. Presdiposisi factors such as age, sex, history of previous illness, etc..
2. Factor triggers, such as exposure by a specific disease agent.
3. Drivers, such as exposure to repeated, heavy workload.
4. Weight factors, such as low income, nutritional status, housing conditions, etc..
D. Exposure and vulnerability
1. Exposure
Exposure is a condition in which the host is in effect or interact with elements of primary and secondary causes or with environmental elements that can encourage the disease process.
2. Susceptibility
Vulnerability is a state in which the host has a condition that easily influenced or interact with elements of the cause to allow the occurrence of disease.
E. Classification of Diseases
WHO since 1984 published several revisions of the book "The International Classification of Diseases (International Clasification of Disease / ICD)
In classification, ICD include 17 main groups based on the cause of the disease with the disease, the nature of disease and location of disease, as follows:
1. Infectious diseases and perasit
2. Neoplasm
3. Endocrine diseases, nutrition, and metabolic and immunity disorders
4. Diseases of blood and blood-forming organs
5. Mental Disorders
6. Diseases of the nervous system and sensory organs
7. Circulatory system diseases
8. Respiratory system diseases
9. Digestive system disease
10. Urinary and genital system diseases
11. Complications of pregnancy, childbirth, and puerperal
12. Skin and subcutaneous tissue
13. System disease of skeletal muscle and connective tissue
14. Kalainan congenital
15. Certain conditions originating from the perinatal period
16. Symptoms, signs, and circumstances that are not clear
17. Injury and poisoning
Each subsequent disease in the classification has some type of disease according to the criteria of symptoms and signs.
1. The disease is the failure of the mechanism of adaptation of organisms to respond appropriately to stimuli or pressures causing interference with the function / structure of the organization or system of the body (Gold Medical Dictionary)
2. Disease is a condition in which the life process are no longer regular or interrupted his journey (Van Dale's Woordenboek der Nederlandse Tell)
Azwar (1988) concluded that the disease is:
A situation where there is disruption of form and function that are in a state that is not normal.
B. Development of Disease Occurrence Theory
At first, the concept is based on the existence of supernatural beings or interruption because of the wrath of the mighty creator.
The development of the theory of the next occurrence of the disease are:
1. Theory Contangion
The occurrence of disease is required contact between one person to another.
2. The theory of Hippocrates
Diseases caused by environmental influences in particular: water, air, soil, weather.
3. Humoral theory
Diseases caused by disorders of fluid balance in the human body.
4. Miasma Theory
Diseases caused by the remnants of living beings who experience decay, thus leaving air pollution and environmental
5. Epidemic Theory
Linking the occurrence of disease with weather and geographic (place)
6. The theory of micro-organism (germ terori)
Germs are considered as a single disease.
7. Nutrition and Resistance Theory
The observation of various epidemiological observations.
8. Environmental Ecology Theory
Humans interact with a variety of factors in certain circumstances and in certain circumstances would cause a specific disease.
C. Cause Compound
The disease has more than one cause, not a single character.
Causative factors are grouped into 4 groups, namely:
1. Presdiposisi factors such as age, sex, history of previous illness, etc..
2. Factor triggers, such as exposure by a specific disease agent.
3. Drivers, such as exposure to repeated, heavy workload.
4. Weight factors, such as low income, nutritional status, housing conditions, etc..
D. Exposure and vulnerability
1. Exposure
Exposure is a condition in which the host is in effect or interact with elements of primary and secondary causes or with environmental elements that can encourage the disease process.
2. Susceptibility
Vulnerability is a state in which the host has a condition that easily influenced or interact with elements of the cause to allow the occurrence of disease.
E. Classification of Diseases
WHO since 1984 published several revisions of the book "The International Classification of Diseases (International Clasification of Disease / ICD)
In classification, ICD include 17 main groups based on the cause of the disease with the disease, the nature of disease and location of disease, as follows:
1. Infectious diseases and perasit
2. Neoplasm
3. Endocrine diseases, nutrition, and metabolic and immunity disorders
4. Diseases of blood and blood-forming organs
5. Mental Disorders
6. Diseases of the nervous system and sensory organs
7. Circulatory system diseases
8. Respiratory system diseases
9. Digestive system disease
10. Urinary and genital system diseases
11. Complications of pregnancy, childbirth, and puerperal
12. Skin and subcutaneous tissue
13. System disease of skeletal muscle and connective tissue
14. Kalainan congenital
15. Certain conditions originating from the perinatal period
16. Symptoms, signs, and circumstances that are not clear
17. Injury and poisoning
Each subsequent disease in the classification has some type of disease according to the criteria of symptoms and signs.
Hospital Management
Fields of hospital management and organizational structure
Management is the process of activities to achieve certain goals through cooperation with others. In this process there are activities of planning, organizing, and supervision.
Management area that need attention are:
1. Planning management
2. Financial management
3. Field of personnel management
4. Biadang hospital information management and medical records
5. Field office management
6. The field of logistics management
7. Bidnag management of pharmaceuticals and generic drugs
8. Field of medical management and care
9. The field of nutrition manajemna
10. Linen management and laundri
11. Field hospital sanitation management and environmental impact
12. Nosocomial infection control management
13. Field of work safety management
14. The field of security management
15. Field marketing management
16. Field monitoring and evaluation management
The division of tasks and organizational structure
In an effort to achieve the target of a hospital must choose an organizational structure that efktif easy to operate and not much bureaucracy. Determination of the organizational structure is intended to be able to divide tasks, provide authority, to supervise and hold accountable.
A successful hospital organizations have cirri:
• organizational structure pyramid-shaped but not flat
• short-tier hierarchy
• organized team oriented malleable and very easy to be dissolved again.
Organizations who served in the hospital are:
• Board of Trustees
• Director of the hospital
• Vice president of medical support
• Deputy director of medical service
• Vice president of promotion and prevention
• Deputy director of general administration and finance
• Head of outpatient
• Head of the emergency room
• Head of hospitalization
• Head of laboratory installation
• Head of radiological installations
• Head of the installation of medical records and information
• Head of administration and staffing
• Head of finance
• Head bookkeeping
• Head of pharmacy
• Head of the hospital facilities maintenance installation
• Head of installation supplies
• Head of the installation of environmental health and occupational health
• Chief operating room and delivery room
• Head UPF diagnostic and physiotherapy
• Committee
Management is the process of activities to achieve certain goals through cooperation with others. In this process there are activities of planning, organizing, and supervision.
Management area that need attention are:
1. Planning management
2. Financial management
3. Field of personnel management
4. Biadang hospital information management and medical records
5. Field office management
6. The field of logistics management
7. Bidnag management of pharmaceuticals and generic drugs
8. Field of medical management and care
9. The field of nutrition manajemna
10. Linen management and laundri
11. Field hospital sanitation management and environmental impact
12. Nosocomial infection control management
13. Field of work safety management
14. The field of security management
15. Field marketing management
16. Field monitoring and evaluation management
The division of tasks and organizational structure
In an effort to achieve the target of a hospital must choose an organizational structure that efktif easy to operate and not much bureaucracy. Determination of the organizational structure is intended to be able to divide tasks, provide authority, to supervise and hold accountable.
A successful hospital organizations have cirri:
• organizational structure pyramid-shaped but not flat
• short-tier hierarchy
• organized team oriented malleable and very easy to be dissolved again.
Organizations who served in the hospital are:
• Board of Trustees
• Director of the hospital
• Vice president of medical support
• Deputy director of medical service
• Vice president of promotion and prevention
• Deputy director of general administration and finance
• Head of outpatient
• Head of the emergency room
• Head of hospitalization
• Head of laboratory installation
• Head of radiological installations
• Head of the installation of medical records and information
• Head of administration and staffing
• Head of finance
• Head bookkeeping
• Head of pharmacy
• Head of the hospital facilities maintenance installation
• Head of installation supplies
• Head of the installation of environmental health and occupational health
• Chief operating room and delivery room
• Head UPF diagnostic and physiotherapy
• Committee
Langganan:
Komentar (Atom)